Beating childhood cancer starts with eating well.
Read our latest report
FoodHeals™: Exploring Nutritional Aspects of Childhood Cancer.
Shedding Light on the Importance of Nutritional Support in Childhood Cancer Care.
Every day we see kids fight cancer with all they’ve got.
But sometimes that’s not enough.
40% of children with cancer in India are malnourished at the time of diagnosis. 100% of them can fight harder with better nutrition. That’s right, there’s hope for every child with cancer.
You help pave their road to recovery. #FoodHeals
With our trained paediatric cancer nutritionists and food aid, we give children fighting cancer a chance at survival. Here’s how…

Enable Hospitals
We partner with government and charity cancer hospitals to provide them with a Paediatric Oncology Nutritionist.

Train Nutritionists
We handpick and train a team that’s big on both heart and skill. They help counsel children with cancer on nutritional choices.

Provide Aid
We provide hot meals, in-meals, nutritional supplements, eggs, bananas, and monthly ration bundles for a family of four.
Our journey starts at a hospital and ends at a playground.
Hear what Dr Krishna from MNJ Hospital, Hyderabad, has to say:
A future full of possibilities starts with a meal full of goodness.
97%
children are more likely to stick with their treatment plan when nutrition is a part of it.
82%
of our patients improved or maintained their nutritional status despite cancer therapy.
Every fighter has a story to tell.
With your help we’ve been able to make cancer a thing of the past for countless children. Read more about their stories and what the future has in store for them.

A few of our supporters...






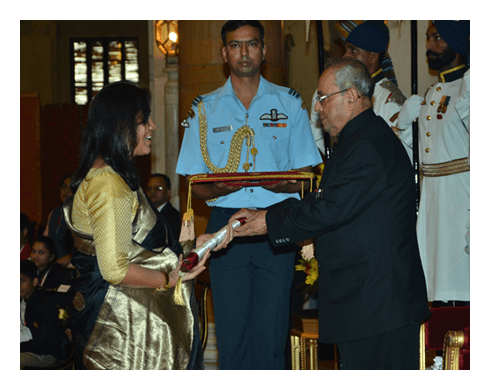
We’ve received love and recognition along the way.
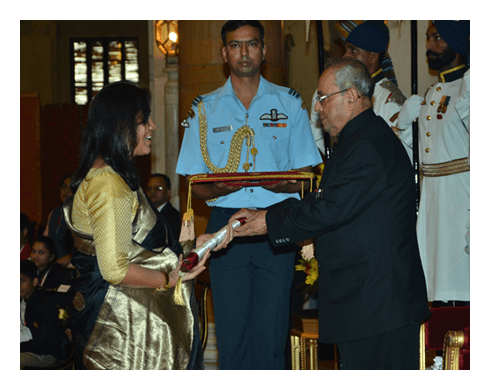
Recipient of the National Award for Child Welfare from the Hon’ble President of India in 2015-16.
Hope delivered.
Even if you can’t support us today, we’d love to keep you in the loop every other week. Join our mailing list.



